By Dr Nick Proctor and Louisa Oliver Byrne, expert-trainers of the Understanding Pharma Market Access in the US course.
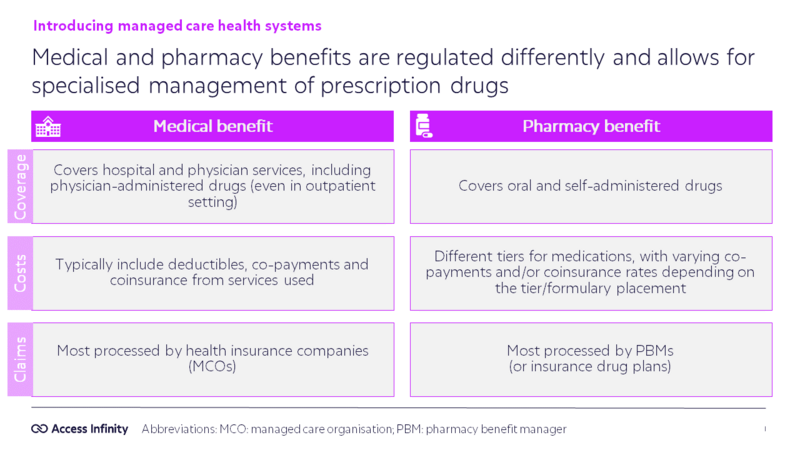
In the United States, access to healthcare is structured into two benefit types: medical and pharmacy.
Key Distinctions Between Medical and Pharmacy Benefits
Both medical and pharmacy benefits serve unique roles in healthcare delivery. The fundamental differences lie in how they are managed, the type of coverage they provide, and how claims are processed.
🏥 Medical Benefits
Medical benefits are designed to cover hospital and physician services. This includes physician-administered drugs – including those administered in an outpatient setting – such as chemotherapy infusions or some vaccines. Managed by medical directors within Managed Care Organisations (MCOs), these benefits typically involve the following:
- Coverage: Encompasses hospital stays, outpatient services, and drugs administered by healthcare providers.
- Costs: Patients usually face deductibles, co-payments, and coinsurance tied to the medical services they use.
- Claims: Most medical benefit claims are processed through health insurance companies (MCOs).
💊 Pharmacy Benefits
Pharmacy benefits, on the other hand, are dedicated to the management of oral and self-administered medications. These benefits are often managed by Pharmacy Benefit Managers (PBMs), third-party entities that specialise in optimising the delivery and cost-efficiency of prescription drugs. The characteristics of pharmacy benefits include:
- Coverage: Focuses on retail prescription drugs, including maintenance medications for chronic conditions like diabetes or hypertension.
- Costs: Often structured around a tiered formulary system. This means patients’ out-of-pocket costs, such as co-payments or coinsurance, depend on the placement of drugs within these tiers.
- Claims: Typically processed through PBMs or private drug plans
⚖️ Managed Care Considerations
Managed care systems are central to balancing the medical and pharmacy benefits for patients and providing a comprehensive health plan to its members. These systems coordinate funding from various sources - government programmes like Medicare and Medicaid, employers, and patients. The differentiation between medical and pharmacy benefits also enables tailored management strategies:
- Medical Benefits: Governed by medical directors and influenced by general healthcare regulations, ensuring services align with clinical care standards at an appropriate cost.
- Pharmacy Benefits: Defined by PBMs and pharmacy directors, who negotiate drug prices and manage formularies to balance cost-benefit.

